how to get medicare to pay for incontinence supplies
The estimated amount of supplies needed per day. Ad 30 Years of Providing Our Customers Superior Value Industry Leading Service.
Incontinence Supplies Through Medicaid Home Care Delivered
Medicare Part B Medical Insurance Part B covers certain doctors services outpatient care medical supplies and preventive services.
. Its rules vary from state to state so you must check from your own states medicaid program if you may get free incontinence supplies or not via medicaid. The type of incontinence products covered and whether theyre covered at all may vary so its a good idea to check with the specific Medicare Advantage plan if this is a benefit youre interested in. You can get started by comparing plans online for free or by calling to speak with a licensed insurance agent.
Usually doesnt cover common medical supplies that you typically use at home like bandages and gauze. Unfortunately Medicare doesnt typically cover absorbent products. Obtain coverage through the Veterans Administration.
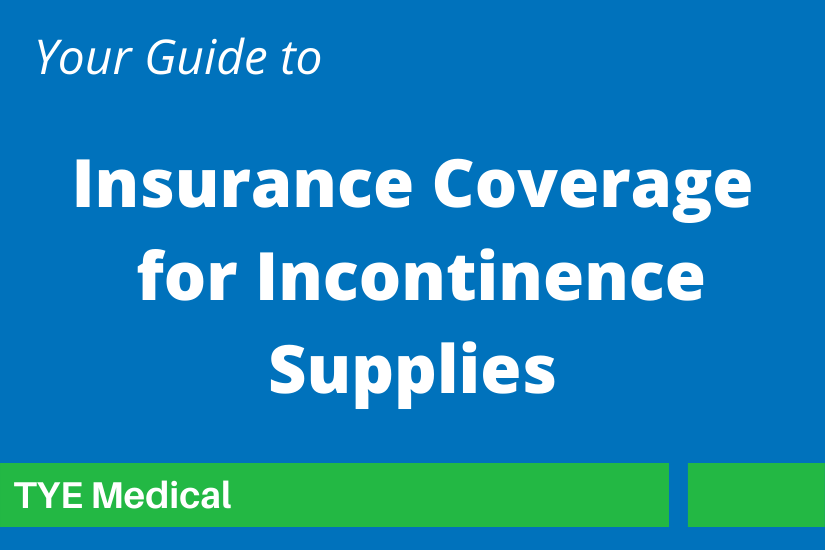
Incontinence Supplies and Medicare Coverage is limited but not impossible. Your Medicare insurance provider may also require prior authorization before your incontinence supplies are approved. Humana Medicare Advantage plans that include coverage of over-the-counter health products may typically charge a coinsurance payment for the product.
Documented proof within the last six months that the items are considered medically necessary by a physician. However Medicare may cover non-absorbent products such as catheters and related products. A physicians prescription with qualifying diagnosis Prior Authorization PA or a LetterCertificate of Medical Necessity LMN.
These plans are required by law to cover everything Original Medicare does but they are allowed to provide additional benefits. No Hassle Return Policy. Medicaid is a state funded largest health sponsored program that allows the people to have free or very cheap health treatment.
Your plan determines if you must order through the Medicare supply catalog. Incontinence Supplies Requirements For California. You will need to work.
Because Medicare does not pay for incontinence products buying them for yourself or someone you care for can get expensive quickly. But some Medicare Advantage plans will. Medicare Advantage combines the benefits of Original Medicare.
Youll want to contact your state Medicaid office or the Medicare Advantage plan to identify your options. While Medicare doesnt cover incontinence supplies Medicaid might. However depending on your financial circumstances and the type of medical insurance you choose the cost of incontinence essentials may be reimbursed or at.
Despite the number of people who live with incontinence traditional Medicare does not cover any incontinence supplies like diapers and pads. Here are some tips for spending less on the products you need. Medicare covers some supplies as durable medical equipment.
Medicare generally doesnt cover incontinence supplies or adult diapers outside of nursing homes. Buy From Online Retailers Today. Some Medicare Advantage Part C plans offer enhanced benefit options for products and services not covered by.
It allows medical supply companies to send you incontinence supplies and bill your Medicaid plan for the cost. Medigap Medicare Supplement insurance plans will not cover disposable incontinence supplies. Medicare Advantage plans are sold by private insurers.
Medicare Advantage plans are offered by private insurance companies approved by Medicare and are required by law to cover everything that is included in Original Medicare coverage except for hospice care which is still covered under Part A. Because Medicare is a national program there is no difference in Medicare coverage between each state. The medical reason for needing supplies.
Ad Browse Our Huge Selection Of Discount Incontinence Pad Products. How Can You Money On Incontinence Supplies. Its basically a prescription that establishes what incontinence products are needed for treatment.
This means that products such as bladder control pads adult briefs diapers pull-ons and others all must be paid for through other means. Buy in bulkPlenty of retailers will sell supplies for less when you purchase a large amount at one time. You may need a physicians order a certificate of medical necessity letter of medical necessity or a copy of your medical records.
An Easy Choice For The 1 In 3 Women Who Experience LBL. If youre eligible for benefits through the VA you may be able to receive free incontinence supplies. In order to obtain coverage for these products youll need to obtain a physicians order or a prescription stating what is needed for treating your incontinence.
All incontinence products must typically be paid for out-of-pocket under Medicare including bladder control pads adult diaperstab-style briefs pull-on underwear and other supplies to help manage incontinence. Unfortunately Medicare does not currently offer coverage for any absorbent incontinent products. A Physicians Order is the most common document required by Medicaid plans for incontinence supply coverage.
While Medicare wont help you pay for your Depends some state Medicaid programs help cover the cost incontinence supplies. How Does Humana Medicare Cover Incontinence Supplies. Depending on the rules of the plan you may have to get the incontinence supplies from a provider contracted with the Medicare Advantage plan.
Original Medicare Parts A and B does not cover incontinence supplies but your loved one may get some supplies covered if she has a Medicare supplemental plan. As described in the Tranquility blog Does Medicaid Cover Incontinence Supplies or Adult Diapers those wishing to obtain incontinence supplies under Medicaid need one of the following. Ad Stay Confident With Poise Pads Liners Designed Specifically For Light Bladder Leakage.
While Original Medicare doesnt cover incontinence supplies some Medicare Advantage plans provide a monthly or quarterly stipend to purchase over-the-counter supplies like adult diapers. Set Up a Personalized Delivery Plan 100 Satisfaction Guaranteed. Some plans will cover incontinence.
The rules for Medicaid are different depending on where you live but most states do provide some form of assistance. Medicare typically does not cover incontinence products. To be approved for incontinence supplies under California Medicaid the below is required.
Those with Medicare and Medicaid can select a Dual-Eligible policy to increase benefits. Contact your local Medicaid office for more information.

Does Medicare Cover Incontinence Supplies Medicarefaq

Contact Information And Websites Of Organizations For Medicare Medicare Elderly Care Organization

How To Save On Incontinence Supplies Original Medicare Won T Cover Retireguide

Free Incontinence Products Guide2free Samples Free Stuff By Mail Get Free Stuff Free Samples By Mail

Does Medicare Cover Catheters What Types Are Covered Medicarefaq Catheter Medicare Health Insurance Benefits

Active Life Medical Products Incontinence Supplies At No Cost With Medi Cal And Medicaid Powered Wheelchair Wheelchair Electric Wheelchair

Cookie Error Fix In 2021 Cookies Health Error

Cats Food Continuon Extra Absorbent Incontinence Bed Pads With Waterproof Liner 10 Pack Cats Food You Can Get Bed Pads Waterproof Liner Incontinence
Medicare And Incontinence Products Home Care Delivered
How Can I Get Free Incontinence Supplies

Incontinence Supplies Insurance Guide 180 Medical
Insurance Coverage For Incontinence Supplies Faq Resource Guide
Insurance Coverage For Incontinence Supplies Faq Resource Guide

Are Incontinence Supplies Covered By Medicaid 180 Medical

Does Medicare Cover Incontinence Supplies In 2022 Read More